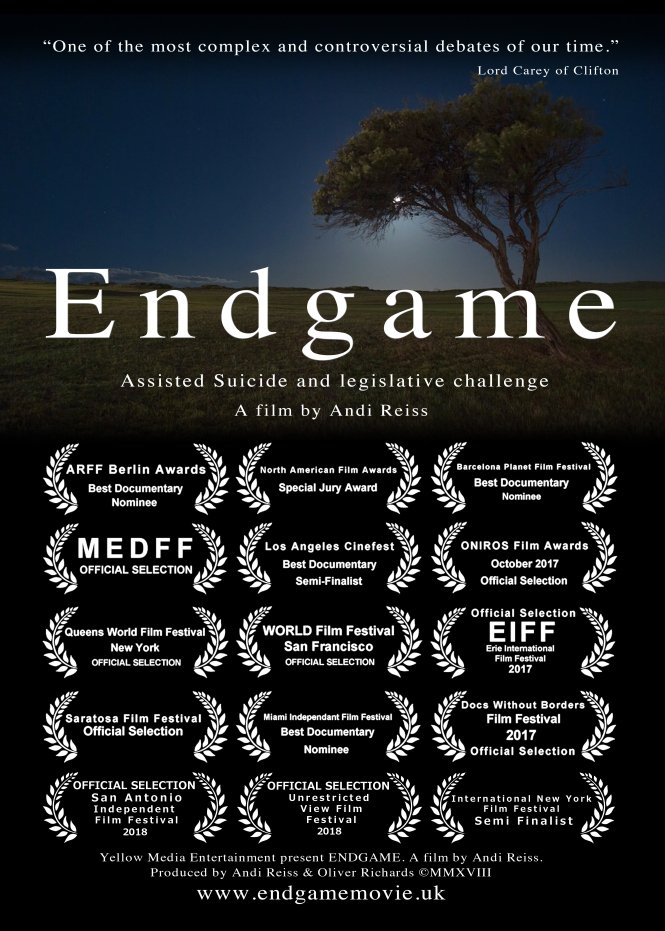
Endgame is a documentary made over 18 months in 2017/8 by independent film maker Andi Reiss. It has been shown, with much praise, at many film festivals and at independent venues. He has now made it available to view on his Vimeo site. A link is embedded at the bottom of this page.
The film, which lasts 65 minutes, follows the stories of Marie, Omid and Alex: three people contemplating a medically assisted suicide in Switzerland. At points the viewing is harrowing and highly emotional – please take that as a warning and have tissues to hand if you watch it!
The documentary asks hard questions and interviews people central to the debate including: Saimo Chahal, (Lawyer for Omid and previously Tony Nicklinson); Richard Huxtable, (Professor of Medical Ethics and Law, Bristol University); Dr Erika Preisig, (Lifecircle) and Rt Rev Lee Rayfield (Bishop of Swindon).
The final section of the film shows Marie and Omid ending their lives at Lifecircle in Switzerland. The in-depth interviews with them immediately prior to them ending their lives are particularly striking. The footage starkly contrasts, on the one hand the joy and gratitude of two people able to peacefully end their suffering after a long period of careful consideration, but on the other hand, the inevitable sadness at loss of life. Omid clearly found happiness in his final interview, the day before he ended his life. The cries of those he left behind speak for themselves.
Another important aspect of the film is that it shows the speed and ease of the intravenous method of medically assisted suicide used at Lifecircle. By controlling a valve, the patient knowingly takes the final step themselves, clearly making this an act of assisted suicide rather than voluntary euthanasia, but because there is no oral ingestion the death is quick and predictable. Dr Preisig has previously told MDMD that using this method the time taken to die is “always the same, 30 seconds to fall asleep, and 4 minutes to die. No coughing, no vomiting, no pain at all”. This contrasts with the possibility of many hours with oral methods, as demonstrated in a recent BBC2 documentary which showed a case in California which took 7.5 hrs.
The tragedy of Omid’s death, which movingly ends the film, is not that Omid chose to end his life. Instead, the tragedy is that Omid’s legal challenge failed and that his eventual medically assisted suicide in Switzerland was so difficult for him to arrange, causing him prolonged suffering he wanted to avoid. It also put his grieving friends and family at risk of prosecution under the UK’s assisted suicide law.
Marie and Omid considered all their alternative options carefully. MDMD strongly advocates good palliative care but recognises that the option of assisted dying is essential for some people for whom even the best palliative alternatives are inadequate.
MDMD’s work will not be complete until this type of peaceful “good death” is integrated into improved palliative care in the UK. Currently the option is only available in the UK to a fortunate and determined few who manage to arrange it in Switzerland. Outsourcing medically assisted dying to another country should only be be seen as a temporary stopgap, pending a compassionate, safe law to permit medically assisted dying for people like Marie, Omid and Alex in the UK, after full and open discussion with their UK doctors. Many of the problems with the current UK arrangement are discussed here and in this study.
Endgame 65 min Oct 2018 from Andi Reiss & Yellow Media Group on Vimeo.






Recent Comments