BBC Radio 4 recently broadcast a 2 part programme about Debbie Purdy. The first part is a dramatisation of the story of how Debbie took her legal case to the House of Lords and as a result caused the director of public prosecutions, (DPP), to issue guidelines clarifying the facts to be considered when deciding whether someone should be prosecuted for assisting suicide. Debbie was concerned that her husband might be prosecuted if he helped her to go to Dignitas in Switzerland, where she could have a medically assisted suicide. (The DPP at the time was Keir Starmer, who is now a front bench Labour MP, and shadow Brexit secretary.) It is 10 years ago this year that Debbie won her case.
In the second part of the programme, The Legacy of Debbie Purdy, Deborah Bowman discusses the issues raised by Debbie’s case with her husband, Omar Puente, her solicitor, Saimo Chahal, and Lord Falconer, the barrister and Labour peer who campaigned on the issue in Parliament.
In recalling the day of the House of Lords ruling on the Purdy case, Lord Falconer said, ‘What Debbie and Omar achieved was absolutely epochal in relation to the struggle because it forced the government, the DPP, to set out what were the circumstances which would lead you to be prosecuted for helping someone to take their own life and what would be the circumstances that would mean you wouldn’t be prosecuted.‘ The resulting DPP guidelines are available here.
The programme raised the recent case of Geoff Whaley, in which his wife, Ann, was interviewed by the police under caution, prior to assisting Geoff to go to Switzerland for a medically assisted death there. The presenter asked ‘Why are friends and family still vulnerable to investigation and potential prosecution given Debbie’s case?‘
Lord Falconer explained that ‘there are still lots of problems because they are dependent on the discretion of the DPP. He decides if there is any bad motivation on the part of the family or friends who helped their loved one take their own life.‘
Asked why his attempts to change the law failed when Debbie Purdy’s case was won, Lord Falconer went on to say ‘I think parliament is totally out of tune with the public’s view… Politicians come into politics to deal with schools and hospitals and issues like that and this is a side issue for them.’
In 2014 Lord Falconer put forward a private member’s Bill in the House of Lords for an assisted dying law along the lines of the Death with Dignity law in Oregon USA. His Bill made significant progress by passing its second reading, but it ran out of time due to the general election of 2015. (Essentially the same Bill was re-introduced in the House of Commons by Rob Marris following the election, but was defeated at its second reading.)
Saimo Chahal, Debbie’s solicitor, went on to represent Tony Nicklinson, who suffered from locked in syndrome. More recently she represented Omid in his legal challenge for assistance to die. She raised the issue of people with degenerative diseases which mean that they would not be helped by the kind of Bill proposed by Lord Falconer as they are not expected to die within six months, but have much longer to suffer. She quoted Lord Neuberger, one of the law lords who ruled in the Nicklinson case, saying surely these people are even more deserving of our sympathy than those who only have a few months to suffer.
Although the Nicklinson and Omid cases failed, the Nicklinson case did help persuade ex Archbishop of Canterbury, Lord Carey to change his view on assisted dying, so that he now supports assisted dying for cases such as these.
Lord Falconer was asked why he proposed a law that would only help those with six months or less to live. He replied ‘Authorising people to assist somebody to die should be limited to those who are dying already. I think that by and large being opposed to helping people to commit suicide is the right policy position for the state to be in, however if you are dying you should have choices as to how you die.‘
The presenter pointed out the medical difficulties of making an accurate life-expectancy prognosis, which Lord Falconer accepted, but said that doctors had to make difficult decisions all the time.
Saimo Chahal agreed with Lord Falconer that there was an underlying principle of personal autonomy over end of life wishes which should be respected, but she said ‘I personally cannot understand why people who have 6 months or less should be helped but not people who have a degenerative condition which is life shortening, who have years and years of pain and agony ahead of them. It seems to me that those very people deserve to have autonomy over when they bring their lives to an end.‘
Lord Falconer responded that ‘the problem is that if suffering becomes the test, you are asking the law to make quite difficult decisions’. He went on to highlight the difficulties with people who are suffering from extreme depression.
Clearly there are difficult decisions to be made – both medical and legal. What seems to be missing is agreed guidelines to tackle them both, while providing adequate protection from those who may be coerced to act against their “true” wishes. It is unfortunate that the programme was not able to explore this point further. It is instructive, for example, to compare the existing right of someone to refuse life-sustaining treatment, or to refuse food and liquid, in order to end their life, but the absence of a right to request medical assistance to die when faced with incurable suffering. Two recent cases highlight this issue, both with motor neurone disease. John King ended his life by removing his ventilator, but Noel Conway’s legal challenge was refused, partly because he has this option of removing his ventilator which he could choose. We should note that the criteria which separate these very similar cases do not involve issues of the risk of coercion, nor any estimate of life-expectancy. Surely it cannot be acceptable to force people to suffer from incurable conditions against their will when they are not dependent on life-sustaining treatment which they could refuse, or where such refusal of treatment could lead to a protracted and unpleasant death.
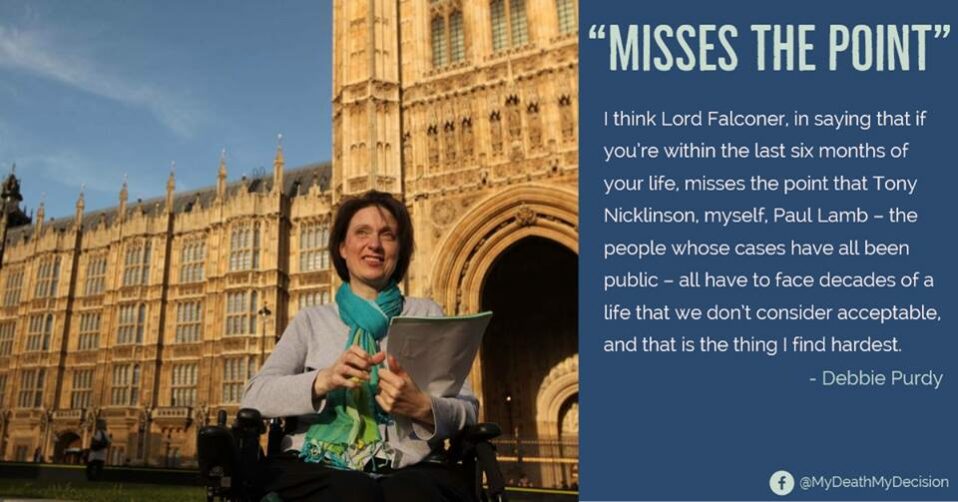
One thing that wasn’t pointed out was that in her final interview Debbie’s views on the six month issue were very clear: ‘I think Lord Falconer, in saying that if you’re within the last six months of your life, misses the point that Tony Nicklinson, myself, Paul Lamb – the people whose cases have all been public – all have to face decades of a life that we don’t consider acceptable, and that is the thing I find hardest.‘ Saimo Chahal was clearly echoing Debbie’s point of view.
Despite these limitations, the programmes are both fascinating. It is particularly helpful to hear a discussion on the issue of the six month criterion – something that MDMD has strong views on.
The progammes are available for a limited time here:







Recent Comments