 For over 50 years, abortion was legal in England, Scotland, and Wales, but not in Ireland or Northern Ireland, leading to a quarter of a million women travelling, often alone, to access it. This type of injustice risks being repeated between England and Wales if Welsh politicians vote down assisted dying proposals – as then, people will need to travel to England to have the procedure on the NHS. Humanists UK and My Death, My Decision are urging politicians to give terminally ill Welsh people the same options and choices that hundreds of thousands of dying people have around the world.
For over 50 years, abortion was legal in England, Scotland, and Wales, but not in Ireland or Northern Ireland, leading to a quarter of a million women travelling, often alone, to access it. This type of injustice risks being repeated between England and Wales if Welsh politicians vote down assisted dying proposals – as then, people will need to travel to England to have the procedure on the NHS. Humanists UK and My Death, My Decision are urging politicians to give terminally ill Welsh people the same options and choices that hundreds of thousands of dying people have around the world.
What is the Legislative Consent Motion (LCM)?
On Tuesday 27 January, members of the Senedd will vote on a Legislative Consent Motion (LCM) relating to the Terminally Ill Adults (End of Life) Bill.
This vote is not about whether assisted dying should be legal in Wales. That decision to change the criminal law will already have been taken at Westminster under reserved powers, where 75% of Welsh MPs voted strongly in favour. Instead, the LCM will determine whether Wales should hold the powers to shape how the law is delivered for the people of Wales.
The LCM concerns a small number of clauses inserted into the Bill to ensure Wales can shape its own implementation of assisted dying. These include:
- Making sure people can give information, have assessments, and get reports in Welsh,
- Letting Welsh Ministers give guidance that fits the needs of Welsh communities,
- Allowing the Welsh Healthcare system (including NHS Wales) to provide assisted deaths,
- Making sure Wales is involved in checking the system and reporting on how it works.
Rejecting the LCM would therefore neither block the law, alter eligibility, nor delay implementation. It would only limit Welsh decision-making on how the law is delivered safely, consistently, and equitably in Wales.
What Happens If the LCM Is Rejected?
 If the Senedd refuses consent, but the Bill passes in Westminster:
If the Senedd refuses consent, but the Bill passes in Westminster:
- The devolved implementation clauses will be removed.
- Assisted dying will still become lawful in Wales.
- Wales will lose the powers needed to build a public service-led, Wales-specific service.
Likely outcomes include:
- Only private firms deliver assisted dying services in Wales for a fee;
- Welsh residents forced to travel to England for assessment and provision;
- No guarantee of Welsh-language access;
- No Wales-specific clinical guidance;
- No tailored oversight reflecting Welsh communities and health needs.
In effect, Wales would lose the ability to design a system rooted in Welsh values, geography, language, and healthcare structures, whilst still being subject to the change in criminal law.
For over 50 years, abortion was legal in England, Scotland, and Wales, but not in Ireland or Northern Ireland, leading to a quarter of a million women travelling, often alone, to access it. This type of injustice risks being repeated between England and Wales if Welsh politicians vote down assisted dying proposals – as then, people will need to travel to England to have the procedure on the NHS. Humanists UK and My Death, My Decision are urging politicians to give terminally ill Welsh people the same options and choices that hundreds of thousands of dying people have around the world.
Who will be most affected: inequality and low incomes in Wales
Multiple reputable organisations, human-rights bodies and peer-reviewed researchers have documented how the abortion ban (and subsequent uneven implementation) in Northern Ireland disproportionately impacted people on low incomes, those living in remote areas, or socially vulnerable people.
Similarly, if assisted dying becomes available only through private providers or by travelling to England, people on lower incomes will face the greatest barriers. Wales has lower average household incomes than most of the UK and higher levels of poverty and long-term illness.
Travel, accommodation, transport of medical equipment, and time away from carers or family impose costs that many households cannot meet. Those already facing financial hardship or in remote communities would be particularly affected.
Ensuring the Senedd retains implementation powers is vital for fairness. Without them, access to assisted dying for Welsh people risks becoming determined by wealth, health, and postcode, deepening existing inequalities.
Welsh voices on assisted dying
74% of Welsh people support a change in the law. Support is broad-based across all major political parties.
 Gemma Williams, from Carmarthenshire, has lived with multiple sclerosis (MS) for more than 20 years. She supports the Terminally Ill Adults (End of Life) Bill and backs terminally ill people having a choice. She said:
Gemma Williams, from Carmarthenshire, has lived with multiple sclerosis (MS) for more than 20 years. She supports the Terminally Ill Adults (End of Life) Bill and backs terminally ill people having a choice. She said:
‘As someone who has lived with MS for over twenty years, I know the importance of feeling safe, respected, and in control of my own care. The safeguards in the Terminally Ill Adults Bill are stronger than anything that exists today, and giving Wales the power to tailor how the law works will protect people like me, not endanger us. No one should be forced to travel, struggle, or suffer simply because they are ill or because they are Welsh. Choice is not a threat, it is dignity.’
Graham Winyard, Board Member of My Death, My Decision, said:
‘If the Senedd rejects these implementation powers, assisted dying will still become legal – but Wales will be left with a system designed elsewhere, for different communities and different needs. That outcome would entrench inequality and deny dying people fair access to a safe, well-regulated service. We urge Welsh politicians to learn from the mistakes of the past and ensure that, this time, no one is excluded by geography, language, or income when making the most personal decision of their lives.’
Notes
Members of the MDMD team, as well as individuals affected by the current law on assisted dying, are available for interview upon request
For further comment or information, media should contact Nathan Stilwell at nathan.stilwell@mydeath-mydecision.org.uk or phone 07456200033. (media only)
Media can use the following press images and videos, as long as they are attributed to “My Death, My Decision”.
My Death, My Decision is a grassroots campaign group that wants the law in England and Wales to allow mentally competent adults who are terminally ill or intolerably suffering from an incurable condition the option of a legal, safe, and compassionate assisted death. With the support of over 3,000 members and supporters, we advocate for an evidence-based law that would balance individual choice alongside robust safeguards and finally give the people of England and Wales choice at the end of their lives.
.



 Baroness Butler-Sloss
Baroness Butler-Sloss 

 We were deeply saddened to hear that John Knight CBE, our esteemed patron, died on 2
We were deeply saddened to hear that John Knight CBE, our esteemed patron, died on 2

 For over 50 years, abortion was legal in England, Scotland, and Wales, but not in Ireland or Northern Ireland, leading to
For over 50 years, abortion was legal in England, Scotland, and Wales, but not in Ireland or Northern Ireland, leading to  If the Senedd refuses consent, but the Bill passes in Westminster:
If the Senedd refuses consent, but the Bill passes in Westminster: Gemma Williams, from Carmarthenshire, has lived with multiple sclerosis (MS) for more than 20 years. She supports the Terminally Ill Adults (End of Life) Bill and backs terminally ill people having a choice. She said:
Gemma Williams, from Carmarthenshire, has lived with multiple sclerosis (MS) for more than 20 years. She supports the Terminally Ill Adults (End of Life) Bill and backs terminally ill people having a choice. She said:
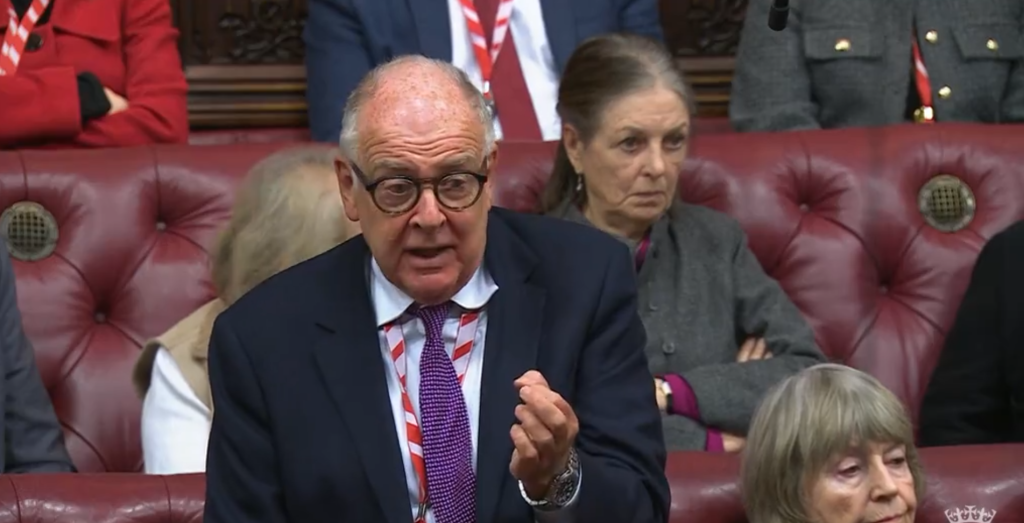
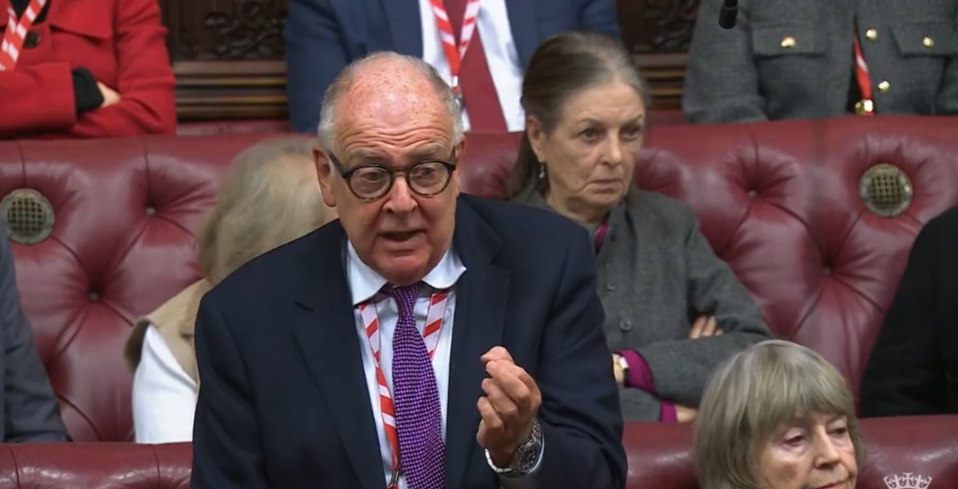
 Lord Kennedy of Southwark, the chief Government whip, said at the end of the debate: ‘We have completed three groups of amendments, which is less than I hoped for… I think that all noble Lords need to reflect on that before we resume our considerations of this Bill next Friday.’
Lord Kennedy of Southwark, the chief Government whip, said at the end of the debate: ‘We have completed three groups of amendments, which is less than I hoped for… I think that all noble Lords need to reflect on that before we resume our considerations of this Bill next Friday.’

 Louise Shackleton, who accompanied her husband to Dignitas in Switzerland for an assisted death, said:
Louise Shackleton, who accompanied her husband to Dignitas in Switzerland for an assisted death, said:








Recent Comments