The House of Lords Select Committee for the Terminally Ill Adults (End of Life) Bill has just announced its final oral witnesses, and it will not hear from terminally ill individuals or those who have assisted loved ones to die. Clare Turner, a terminally ill person, and Louise Shackleton, who accompanied her husband to Switzerland for an assisted death, have deemed this omission ‘outrageous’. Humanists UK and My Death, My Decision say this is an unbelievable omission that completely undermines the Committee’s work.
It has been reported that the Committee is weighted against assisted dying, with more opponents of legislation change than supporters. Analysis by Humanists UK and My Death, My Decision suggests that the experts so far called to give evidence consist overwhelmingly of those opposed to assisted dying. Apart from the Bill sponsors and ministers, those called to give evidence consist of three people supportive of assisted dying, nine against, and 20 neutral.

EDITORIAL USE ONLY Louise Shackleton Picture date: Thursday May 15, 2025. PA Photo. Belinda Jiao/PA Media Assignments
Louise Shackleton, who was investigated for 10 months for accompanying her husband, Anthony, to Switzerland for an assisted death, said:
‘This is outrageous. I was investigated by the police for holding my husband’s hand as he died in Switzerland. Now the Lords won’t even hold space to hear from people like me. The law criminalised our love, and now the Lords Committee has silenced our evidence.
‘The state forced me to fly thousands of miles with my dying husband, Anthony, so he would not die alone, for mercy. He wanted this, he wanted choice, control, and peace at the end of his life. Did he not deserve that? The police then treated me like a suspect for being with him and supporting him in his own decision. How is that experience not vital evidence?’
 Clare Turner, a mother of two with stage four breast cancer, said:
Clare Turner, a mother of two with stage four breast cancer, said:
‘I feel very betrayed by this Committee. They have heard from lawyers and opponents, but not from those who would actually qualify under this Bill. As a woman who will, I deserve to be in the room. Excluding us silences the very evidence they claim to seek.
‘I’m not fearful about death, but without assisted dying, I feel fearful about the actual dying process. I want my daughters to have a positive lasting memory of me, and being able to choose the timing, nature, and location of that death would give me and my family incredible peace. I would like to die under the lovely oak tree in my garden, surrounded by the people I love. If the law doesn’t pass, people like me will be denied that choice.’
Who has been called to provide evidence?
The Select Committee has called 36 witnesses to give evidence.
Of them, excluding the Bill sponsors and Government ministers, only three are supportive of a change in the law: Professor Sam Ahmedzai, Professor Tom Shakespeare, and Sir Nicholas Mostyn KC. Nine of the witnesses have a personal negative opinion about the Bill, or represent organisations that have strongly opposed the Bill. The remaining witnesses take a neutral stance.
10 of the witnesses had already given evidence to the Bill Committee in the House of Commons back in February. The Commons Bill Committee heard from the wife of a terminally ill British man who had an assisted death in Spain; the sister of a man who had an assisted death in Queensland, Australia; and the brother of a British woman with motor neurone disease who travelled to Dignitas in Switzerland for an assisted death.
We do not see why the Lords Committee did not likewise want to hear directly from those with personal testimonies.
No international evidence, either
One of the opponents of the Bill, Lord Goodman, wrote in the Times yesterday:
‘I’m a member of the select committee set up to probe the bill’s potential implementation and effects. Hence my internet search. The bill would provide for assisted suicide under certain circumstances, and I wanted to find out more about how it works abroad.’
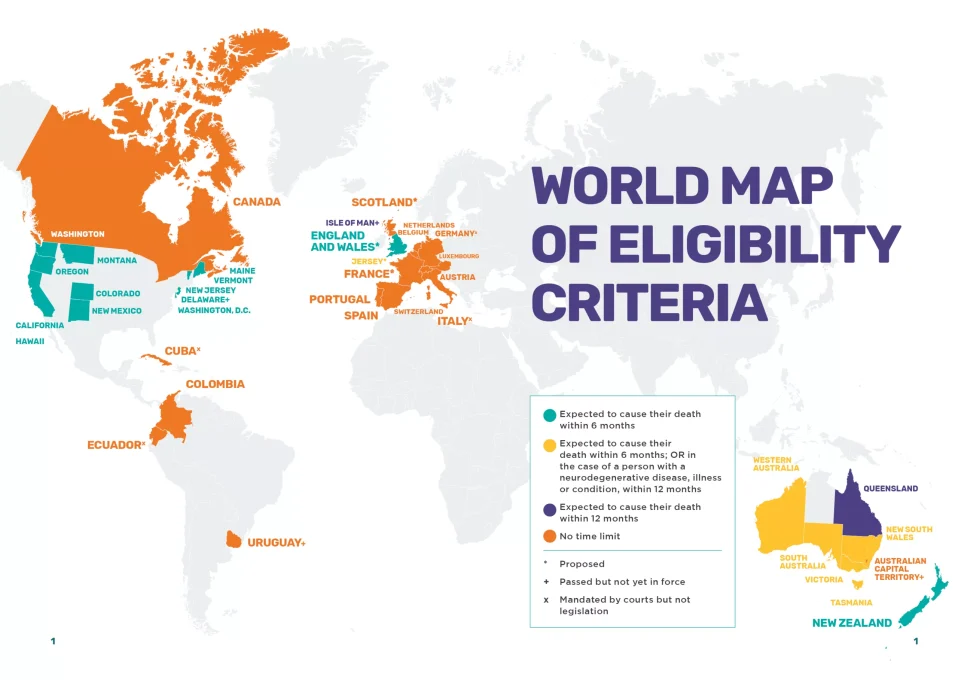
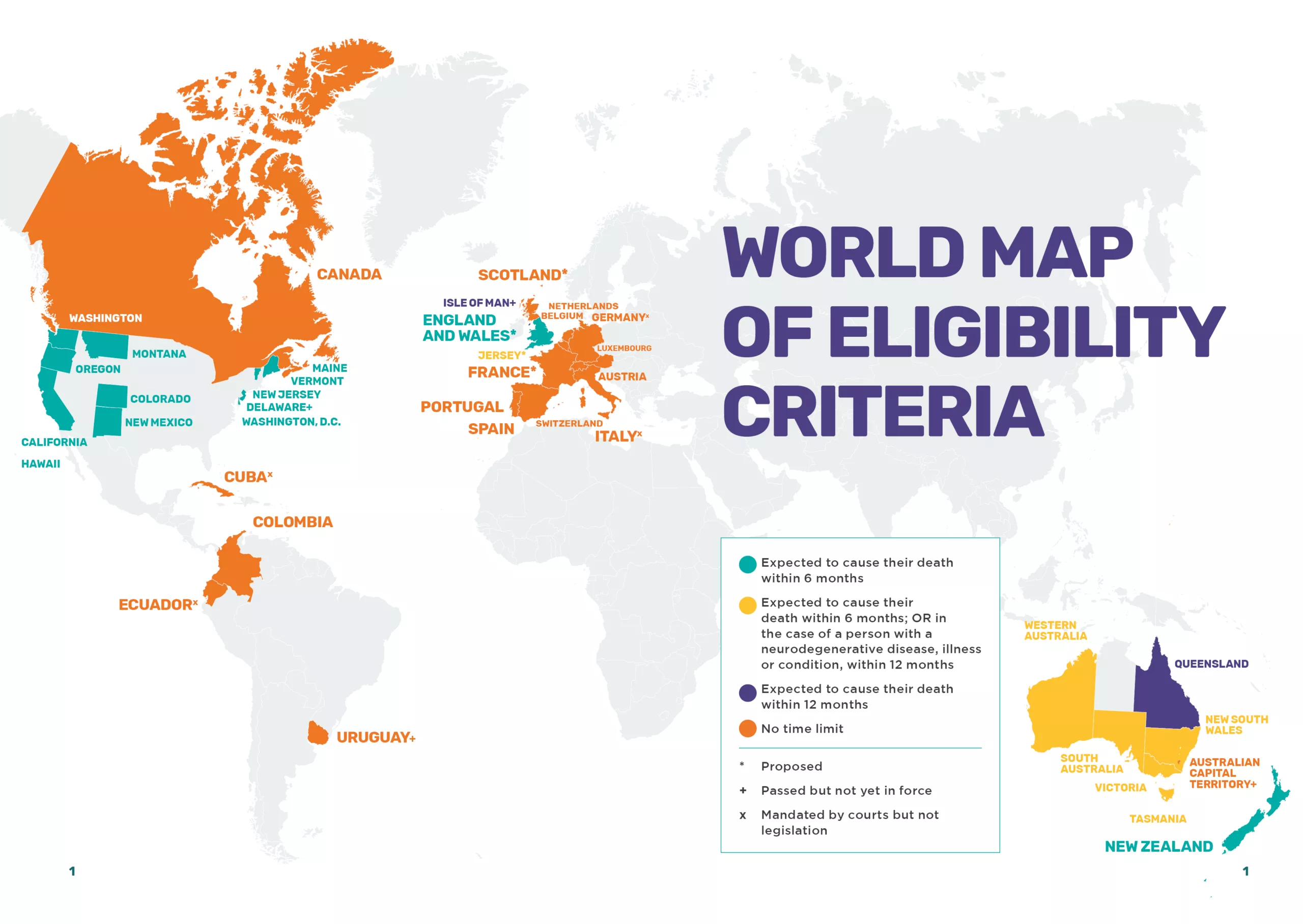
This is ironic because the Committee did not request evidence from any international experts, including those from jurisdictions where assisted dying is working. This month, Uruguay became the 34th jurisdiction in the world to allow assisted dying.
The House of Commons Bill Committee received evidence from international witnesses at the start of this year. Experts from Australia and the United States told the committee that assisted dying was working safely and compassionately in their respective jurisdictions. The Health and Social Care Committee inquiry into assisted dying also took oral evidence from a range of international experts in 2023. Furthermore, New Zealand, Western Australia and Victoria have produced detailed annual reports and reviews that show their respective laws are safe and compassionate.
Dave Sowry, Board Member of My Death, My Decision, accompanied his wife to Switzerland for an assisted death in 2022. He said:
‘Listening to the questions asked by the House of Lords committee taking evidence about the Terminally Ill Adults Bill, you might not realise that this Bill is about terminally ill adults at the end of life who want a simple, safe process to reassure them as they live out their last weeks. These people must be put at the centre of every discussion at every step of the process, and their autonomy must be respected. Why aren’t their views being heard by the committee?
‘Instead, we’ve heard old arguments rehashed for no apparent reason other than to slow the Bill down. None of these arguments are different to the concerns raised in the debates that preceded the introduction of similar laws in jurisdictions with a terminal illness, mental capacity model. In these jurisdictions, this model now operates successfully and safely. Why hasn’t this evidence from abroad been allowed to be heard in Committee?’
Richy Thompson, Director of Public Affairs and Policy at Humanists UK, said:
‘It is unbelievable that not a single session for the Terminally Ill Adults Bill Committee will include terminally ill people. You cannot exclude their voices in this debate, and their experience is vital in understanding the workability of the proposed Bill.
‘What is crystal clear is that the status quo is unworkable; it leads to unnecessary suffering, painful suicides, and people fleeing their own country to take control of their deaths. We hope that peers recognise and listen to the lived experience of the terminally ill and understand why the law must change.’
Notes
Members of the MDMD team, as well as individuals affected by the current law on assisted dying, are available for interview upon request
For further comment or information, media should contact Nathan Stilwell at nathan.stilwell@mydeath-mydecision.org.uk or phone 07456200033. (media only)
Media can use the following press images and videos, as long as they are attributed to “My Death, My Decision”.
My Death, My Decision is a grassroots campaign group that wants the law in England and Wales to allow mentally competent adults who are terminally ill or intolerably suffering from an incurable condition the option of a legal, safe, and compassionate assisted death. With the support of over 3,000 members and supporters, we advocate for an evidence-based law that would balance individual choice alongside robust safeguards and finally give the people of England and Wales choice at the end of their lives.



 The House of Lords Select Committee on the Terminally Ill Adults (End of Life Bill) held their second day of oral evidence, where it heard evidence from the Royal College of Psychiatrists (RCPsych) and British Association of Social Workers, and then held a session focused on the role of coroners and medical examiners in assisted deaths.
The House of Lords Select Committee on the Terminally Ill Adults (End of Life Bill) held their second day of oral evidence, where it heard evidence from the Royal College of Psychiatrists (RCPsych) and British Association of Social Workers, and then held a session focused on the role of coroners and medical examiners in assisted deaths. During the session, Dr Annabel Price, College Lead for the Bill at Royal College of Psychiatrists, was challenged by Committee members about the College’s recent arguments against assisted dying. Lord Markham raised concerns, saying:
During the session, Dr Annabel Price, College Lead for the Bill at Royal College of Psychiatrists, was challenged by Committee members about the College’s recent arguments against assisted dying. Lord Markham raised concerns, saying: The second session focused on a technical clause of the Bill, clause 38, which relates to the investigations of deaths after an assisted death. The evidence focused on whether a coroner or a medical examiner should investigate all assisted deaths.
The second session focused on a technical clause of the Bill, clause 38, which relates to the investigations of deaths after an assisted death. The evidence focused on whether a coroner or a medical examiner should investigate all assisted deaths.  Who else will provide evidence?
Who else will provide evidence?
 The Bill sponsor in the Commons, Kim Leadbeater MP, told the Committee:
The Bill sponsor in the Commons, Kim Leadbeater MP, told the Committee:
 Uruguay’s Senate has approved the ‘Dignified Death’ law, making the country the 34th jurisdiction in the world to allow assisted dying. My Death, My Decision is hailing this historic moment, and is calling on the House of Lords to constructively work on the Terminally Ill Adults Bill, so dying Brits can face the same choices as Uruguayans.
Uruguay’s Senate has approved the ‘Dignified Death’ law, making the country the 34th jurisdiction in the world to allow assisted dying. My Death, My Decision is hailing this historic moment, and is calling on the House of Lords to constructively work on the Terminally Ill Adults Bill, so dying Brits can face the same choices as Uruguayans. 
 Welsh patients could be forced to pay privately for assisted dying unless the next Welsh Government ensures NHS provision, according to a report published by the Welsh Parliament today. The Welsh Parliament Health and Social Care Committee Report on the
Welsh patients could be forced to pay privately for assisted dying unless the next Welsh Government ensures NHS provision, according to a report published by the Welsh Parliament today. The Welsh Parliament Health and Social Care Committee Report on the  Graham Winyard, Director of My Death, My Decision, said:
Graham Winyard, Director of My Death, My Decision, said:
 The House of Lords has set up a Select Committee to examine assisted dying in a historic first as the Bill passed its Second Reading in the Lords, a critical stage of the Bill’s passage into law. No such committee has ever been created for a Private Member’s Bill that originated in the Commons, and this has happened just once for government legislation.
The House of Lords has set up a Select Committee to examine assisted dying in a historic first as the Bill passed its Second Reading in the Lords, a critical stage of the Bill’s passage into law. No such committee has ever been created for a Private Member’s Bill that originated in the Commons, and this has happened just once for government legislation. Juliette Sykes, widow of Tim Sykes who died of oesophageal cancer in 2021, attended Parliament today. She said:
Juliette Sykes, widow of Tim Sykes who died of oesophageal cancer in 2021, attended Parliament today. She said: 
 My Death, My Decision has
My Death, My Decision has 
 The Terminally Ill Adults (End of Life) Bill has completed the first day of its Second Reading in the House of Lords, a key stage of the Bill’s passage into law. The debate will continue on Friday 19 September.
The Terminally Ill Adults (End of Life) Bill has completed the first day of its Second Reading in the House of Lords, a key stage of the Bill’s passage into law. The debate will continue on Friday 19 September.



 Kim Leadbeater MP, sponsor of the Terminally Ill Adults (End of Life) Bill Committee, said:
Kim Leadbeater MP, sponsor of the Terminally Ill Adults (End of Life) Bill Committee, said: Silvan Luley, board member of DIGNITAS, the Swiss assisted dying centre, said:
Silvan Luley, board member of DIGNITAS, the Swiss assisted dying centre, said: Notes:
Notes:


Recent Comments