
CC BY-NC-ND 2.0 DEED Attribution-NonCommercial-NoDerivs 2.0 Generic
Sir Keir Starmer, leader of the Labour Party, has pledged a vote on assisted dying in the next parliament if they are to win the next general election. My Death, My Decision welcomes this commitment, which could see assisted dying legalised in the term of the next Parliament.
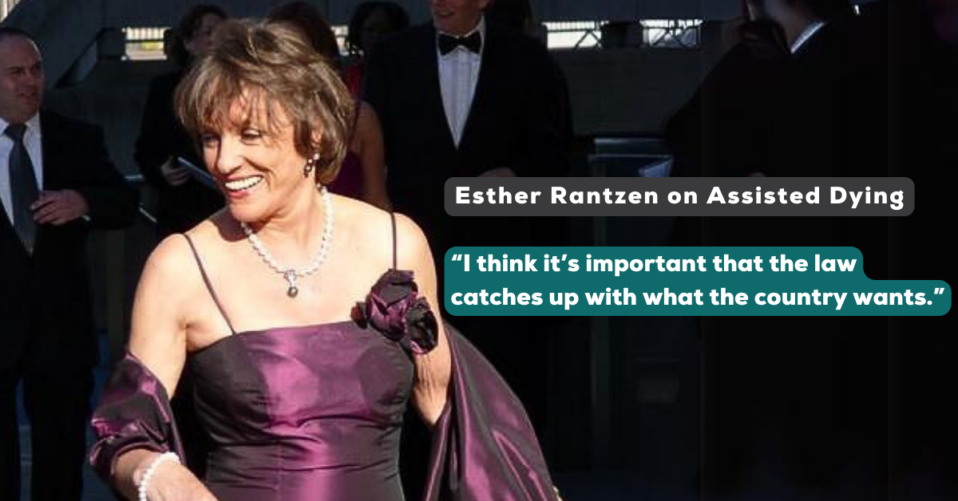
Sir Keir made the commitment when speaking in a phone call with broadcaster Dame Esther Rantzen, who announced in December that she had joined the Swiss assisted dying centre Dignitas.
Sir Keir told Esther: “I’m personally in favour of changing the law… I think we need to make time. We will make the commitment. Esther, I can give you that commitment right now.”

Picture by Andrew Parsons / No 10 Downing Street
When asked whether he’d like a vote to take place within the next parliament, Sir Keir replied: “Oh yes, definitely. I think Esther would agree with this.
“For people who are going through this or are likely to go through it in the next few months or years, this matters hugely and delay just prolongs the agony.”
Trevor Moore, Chair of My Death, My Decision said:
“Sir Keir Starmer’s commitment to give time for an assisted dying debate in Parliament is huge progress towards more compassionate end-of-life choices for people suffering intolerably from incurable conditions. My Death, My Decision welcomes this bold statement – assisted dying law reform is long overdue.
Voters from all parties desperately want the law change to change. It’s about time we stopped exporting compassion to Switzerland and gave people control of their lives and ultimately their deaths”
The Prime Minister, Rishi Sunak, has said he would support allowing enough parliamentary time for a meaningful debate and vote on assisted dying. Mr Sunak also pledged to introduce assisted dying laws if parliament wanted to change the law, saying the government would “facilitate” it in a “legally effective” way.
There has not been a vote on assisted dying since 2015. The most recent attempt to change the law ended when the bill ran out of time in 2021. There are currently no votes or debates expected on this topic in this parliamentary term.
The Health and Social Care Committee recently published its report on assisted dying. The report contained no direct recommendations for legislative change, but clearly outlines the evidence and should be used as a roadmap for the next parliament to legislate on assisted dying.
Progress on assisted dying legislation is being made in Scotland, Jersey and the Isle of Man. Each jurisdiction is due to debate the issue this year. Westminster can learn much from them.
Notes:
Members of the MDMD team, as well as individuals affected by the current law on assisted dying, are available for interview upon request
For further comment or information, media should contact Nathan Stilwell at nathan.stilwell@mydeath-mydecision.org.uk or phone 07456200033.
My Death, My Decision is a grassroots campaign group that wants the law in England and Wales to allow mentally competent adults who are terminally ill or intolerably suffering from an incurable condition the option of a legal, safe, and compassionate assisted death. With the support of over 3,000 members and supporters, we advocate for an evidence-based law that would balance individual choice alongside robust safeguards and finally give the people of England and Wales choice at the end of their lives.
Read more about our work with the Assisted Dying Inquiry: https://www.mydeath-mydecision.org.uk/2023/07/13/our-summary-the-assisted-dying-inquiry/



 The special Oireachtas committee on assisted dying in the Republic of Ireland is set to recommend that legislation should be introduced to allow terminally ill people the right to a dignified death on their own terms. My Death, My Decision welcomes this news, adding to the cases of Scotland, Isle of Man and Jersey in shining a spotlight on the lack of progress at Westminster.
The special Oireachtas committee on assisted dying in the Republic of Ireland is set to recommend that legislation should be introduced to allow terminally ill people the right to a dignified death on their own terms. My Death, My Decision welcomes this news, adding to the cases of Scotland, Isle of Man and Jersey in shining a spotlight on the lack of progress at Westminster.

 Today, the
Today, the 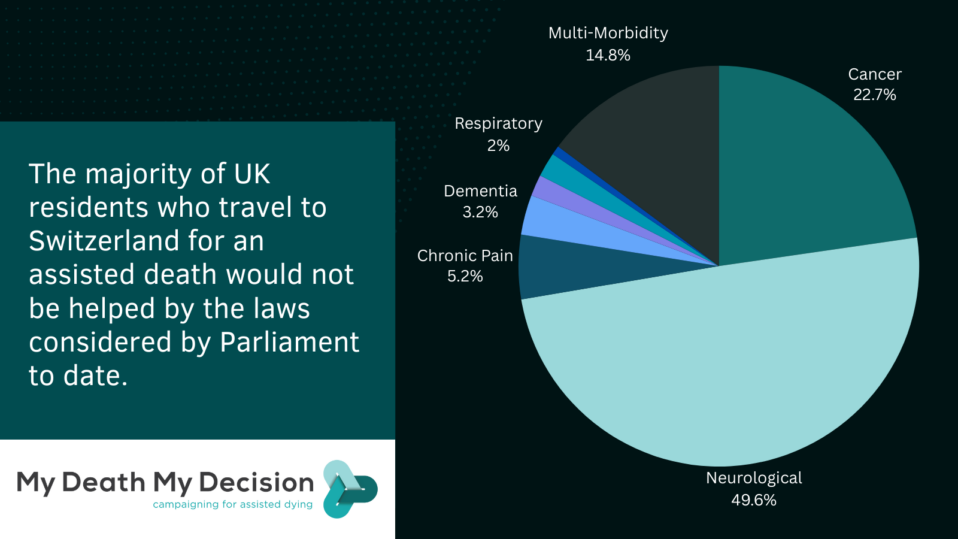
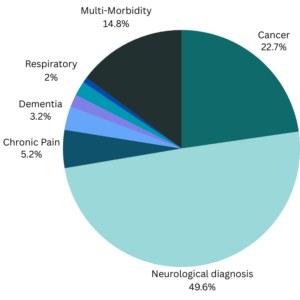 Table 2 UK Residents with neurological diagnoses receiving an assisted death in Switzerland
Table 2 UK Residents with neurological diagnoses receiving an assisted death in Switzerland


 An “ethics review” of assisted dying in Jersey has been published, but campaigners have questioned the need for the review, the scope of the report and the report’s recommendations.
An “ethics review” of assisted dying in Jersey has been published, but campaigners have questioned the need for the review, the scope of the report and the report’s recommendations.
 Dr Alex Allinson’s Assisted Dying Bill has passed its second reading in the Isle of Man Parliament, bringing the jurisdiction a vital step closer to a working, compassionate assisted dying law. My Death, My Decision, whose local Isle of Man branch has been campaigning strongly for a law, welcomes this important step.
Dr Alex Allinson’s Assisted Dying Bill has passed its second reading in the Isle of Man Parliament, bringing the jurisdiction a vital step closer to a working, compassionate assisted dying law. My Death, My Decision, whose local Isle of Man branch has been campaigning strongly for a law, welcomes this important step.

 Over on
Over on 



Recent Comments