 My Death, My Decision is a grassroots campaign group that wants the law in England and Wales to allow those who are terminally ill or intolerably suffering the option of a legal, safe, and compassionate assisted death.
My Death, My Decision is a grassroots campaign group that wants the law in England and Wales to allow those who are terminally ill or intolerably suffering the option of a legal, safe, and compassionate assisted death.
With over 3,000 supporters, we advocate for an evidence-based law that would balance individual choice alongside robust safeguards and finally give people a choice at the end of their lives.
We have long called for an inquiry into assisted dying here in the UK. In 2021, along with Humanists UK, renowned neurosurgeon Dr Henry Marsh and over 50 MPs and peers, we organised a joint letter calling for an inquiry into this vital issue.
The Health and Social Care Committee launched an inquiry into assisted dying in January and at the start of July the Committee held its final oral evidence session. The inquiry will then produce a report, which we expect it to publish around September. It could contain recommendations or even call for a law.
 What happened?
What happened?
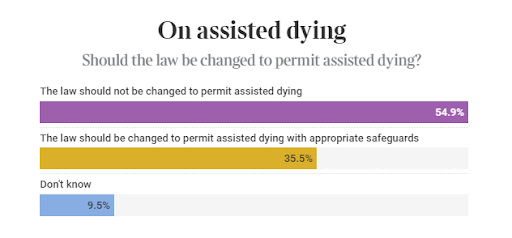
Firstly, the public was invited to participate in a survey, which received 63,000 responses. The Committee has released a partial summary of the survey results, revealing that 94% of respondents believed that “reducing suffering” was a significant factor in their opinion that the current law is wrong.
We submitted written evidence along with over 300 organisations, experts, and individuals.
Additionally, two closed-door roundtable discussions were held with individuals affected by the current law on assisted dying, these included doctors, surgeons, nurses, terminally ill people, disabled people and people who had accompanied loved ones to Switzerland.
The Committee held five oral evidence sessions, during which a variety of domestic and international experts provided testimony and answered questions.
What went right?
The international evidence received was outstanding and informative. Switzerland has allowed assisted dying for over 80 years, the US state of Oregon for 25, Belgium and the Netherlands for over 20. There are also now 28 jurisdictions around the world that allow assisted dying under some criteria. There is a massive wealth of data and experience about assisted dying that can help the UK draft a compassionate law.
MPs on the Committee heard that internationally, end-of-life care improves dramatically after the introduction of assisted dying legislation. James Downar, an expert on Palliative Care from Canada, said that his country had seen ‘the strongest growth of palliative care in its history’ since assisted dying was legalised. Experts from Belgium and the Netherlands said that legalisation had been linked to palliative care, and both countries saw massive boosts in end-of-life care after the law’s introduction.
Overall, the oral evidence sessions showed that assisted dying legislation abroad has led to more compassion, more dignity, better safety and better scrutiny.
What did the inquiry get wrong?
It was clear from the start that an inquiry into the biggest ethical issue of our generation, where many individuals hold extremely strong views, would be an incredibly difficult task. The Committee is concurrently running inquiries into dentistry, pharmacy and future cancers, so there is a lot on their plate.
Despite the good effort, five evidence sessions were always going to leave out key stakeholders. However, the whole reason we are having this debate in the first place, is that many people are living in tremendous pain, suffering and indignity. In our opinion, these people and their friends and loved ones were not given enough weight and should have had a publicly televised oral evidence session for those who wished to share their experiences with a wider audience.
It’s easy to jump straight to philosophical ethical questions, or experts on palliative care, but that is not the reason this topic is so important. The reason we are having this discussion is that grassroots movements like ours are filled with people who are put in barbaric and inhumane situations because we don’t have an assisted dying law.
Secondly, only palliative care doctors were invited to give publicly televised oral evidence. The oral evidence sessions carry a lot of weight; it’s a chance to convince MPs in person and allows MPs to ask in-depth questions. This leaves out surgeons, GPs, psychiatrists, nurses, social workers and many other individuals who will clearly be involved in the assisted dying process and would have vital evidence to share. These groups could only submit evidence in writing or attend the anonymised roundtables.
How could the inquiry have done better?
Many of the MPs on the Committee had previously opposed assisted dying. This doesn’t mean their minds haven’t changed since the vote in 2015, or that the inquiry itself couldn’t change their minds, but the opponents to assisted dying should have declared their views right from the start.
From information in the public domain, it seems several members of the Committee are far more religious than the public at large too, and while that doesn’t automatically mean they oppose assisted dying, they should declare that their religiosity may influence the debate. The same can be said of some contributors to televised evidence sessions, one did not declare they were the Vice President of the Catholic Union before giving testimony. Another had signed an open letter opposing abortion in Northern Ireland under religious groups.
Secondly, while it’s evident that opposing views were always going to be heard in this inquiry, there wasn’t enough effort to challenge falsehoods or exaggerations. A clear example is Canada. In one session, a professor from the USA claimed that people in Canada had been forced into euthanasia by pressure from their families. This claim was repeated in a later evidence session. This is not true. There is no evidence that families have pressured their loved ones into having an assisted death. If someone makes such a bold assertion, the nature of an inquiry is that they should be challenged to give evidence to support their claims.
What next?
The inquiry will write a report which may contain recommendations to the Government, which will be published this year. We expect it to be published around September or October, but there is no set timeline. The Government is then expected to respond.
However, we are doubtful that the report will produce any recommendations, which would be a missed opportunity. We suspect this is the case due to the range of opposition to assisted dying from the committee members.
If a neutral report without recommendations is produced, the next step could be a Citizens’ Jury. Citizens’ juries (also known as assemblies or conventions) have been held on assisted dying in Jersey and France and led to positive, ethical discussions about end-of-life care. These juries bring together everyday citizens to learn and discuss key issues. They have been held all over the world, on issues like climate change, drug use and other ethical issues. They are a great opportunity to let the people have a clear, detailed say on key discussions.
The first oral evidence session included an expert advisor and academic who helped the Citizens’ Jury on assisted dying in Jersey. Dr Mullock told the inquiry: ‘I think it is a very good process and a really good way to have democratic participation.’
The survey, to which 63,000 people responded, asked individuals if they thought a Citizens’ Jury could be a good way forward. The Committee has not yet revealed how many individuals ticked that box.
Trevor Moore, Chair of My Death, My Decision, said:
“We are desperate to see the final report that the committee produces. We hope it takes into account the tremendous international evidence that supports a change in the law and truly understands the scale of unnecessary pain and suffering that exists in the UK because of our current legislation.
If the report contains no set recommendations, the Government should set up a Citizens’ Jury. This would be a vital step in giving the people their say on this crucial issue. Assisted dying gives people back their fundamental right to end their suffering if it gets too much. No one should be forced to endure torturous conditions when the international evidence has shown that compassionate alternatives are available.”
Notes:
Members of the MDMD team, as well as individuals affected by the current law on assisted dying, are available for interview upon request
For further comment or information, media should contact Nathan Stilwell at nathan.stilwell@mydeath-mydecision.org.uk or phone 07456200033.


 My Death, My Decision is a grassroots campaign group that wants the law in England and Wales to allow those who are terminally ill or intolerably suffering the option of a legal, safe, and compassionate assisted death.
My Death, My Decision is a grassroots campaign group that wants the law in England and Wales to allow those who are terminally ill or intolerably suffering the option of a legal, safe, and compassionate assisted death.  What happened?
What happened?

 The Isle of Man took a step closer to introducing an assisted dying law today, as Dr Alex Allinson’s Assisted Dying Bill passed its first reading. The progress being made there, in Scotland and in Jersey shines a spotlight on Westminster, where the Health and Social Care Committee continues its inquiry into assisted dying.
The Isle of Man took a step closer to introducing an assisted dying law today, as Dr Alex Allinson’s Assisted Dying Bill passed its first reading. The progress being made there, in Scotland and in Jersey shines a spotlight on Westminster, where the Health and Social Care Committee continues its inquiry into assisted dying.

 A majority of Surgeons support assisted dying, according to
A majority of Surgeons support assisted dying, according to 







Recent Comments